Chapter 10: Healthier eating
Updated 9 November 2021
This guidance is issued jointly by the Department of Health and Social Care, the Welsh Government, the Department of Health Northern Ireland, Public Health England, NHS England and NHS Improvement, and with the support of the British Association for the Study of Community Dentistry.
Delivering Better Oral Health has been developed with the support of the 4 UK Chief Dental Officers.
Whilst this guidance seeks to ensure a consistent UK-wide approach to prevention of oral diseases, some differences in operational delivery and organisational responsibilities may apply in Wales, Northern Ireland and England. In Scotland the guidance will be used to inform oral health improvement policy.
Diet in the UK
A healthy diet is important for oral and general health. Surveys consistently highlight that the population of the United Kingdom is eating too many ‘free sugars’ (see below), too much saturated fat and salt, and not enough fruit, vegetables, fibre and oily fish.
Defining free sugars
The term ‘Free sugars’ includes all sugars (monosaccharides and disaccharides) added to foods and drinks by the manufacturer, cook or consumer, as well as sugars naturally present in honey, syrups, smoothies, and fruit juices.
It does not include sugars found naturally in whole fresh fruit and vegetables and those naturally present in milk and milk products.
Also included as free sugars are the following:
- all the sugars naturally present in fruit and vegetable juices, concentrates, smoothies, purées, pastes, powders and extruded fruit and vegetable products
- all sugars in drinks except for lactose and galactose naturally present in milk and other dairy-based drinks including:
- all sugars in unsweetened fruit and vegetable juices, fruit and vegetable juice concentrates and smoothies
- all sugars in alcoholic drinks
- all sugars naturally present in dairy-alternative drinks such as soya, rice, oat and nut-based drinks
- lactose and galactose added as an ingredient to foods or drinks, including lactose in whey powder.
Sources: Scientific Advisory Committee on Nutrition, 2015[footnote 1]; Swan and others, 2018[footnote 3]; NHS Eatwell Sugar: the facts, 2019
Some people choose not to have milk and dairy products in their diet for a variety of reasons, for example, if they are unable to digest lactose (lactose intolerance), have an allergy to cow’s milk protein or are following a vegan diet. There are a number of plant-based foods and drinks now available on the market, which can contain free sugars and individuals are advised to look at the labelling and choose unsweetened (lower sugar) versions and those which are fortified with vitamins and minerals such as calcium.
Free sugars in the diet
Free sugars, if consumed, should only be consumed in small amounts. It is recommended that the average population intake of free sugars should not exceed 5% of total dietary energy for age groups from 2 years upwards[footnote 1]. The recommended upper ‘threshold’ of free sugars intake, by age, is presented in Figure 10.1 below and can be accessed on the NHS Change4Life website.
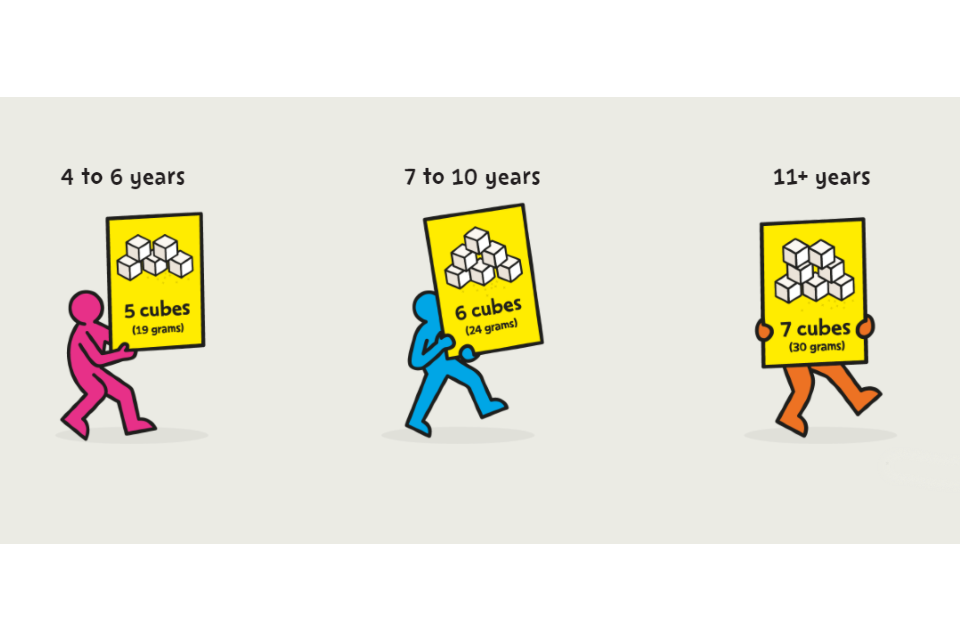
Figure 10.1. Visualisation of sugar recommendations: recommended maximum threshold. One cube is 4g of sugar. Source (2)
| Age | Maximum daily amounts of added sugar |
|---|---|
| 4 to 6 years | 5 cubes (19 grams) |
| 7 to 10 years | 6 cubes (24 grams) |
| 11 years and over | 7 cubes (30 grams) |
In 2016 to 2019, free sugars intake exceeded the government recommendation of providing no more than 5% of total energy intake[footnote 4]. Amongst children and young people, girls aged 11 to 18 years and boys aged 4 to 10 years had the highest mean free sugars intakes as a percentage of total energy (12.5% and 12.4% of total energy respectively); whilst children aged 1.5 to 3 years had the lowest mean intake (9.7%)[footnote 4].
Amongst adults, the reported mean intake of free sugars, as a percentage of total energy intake, was 9.9% for those of working age (19 to 64 years) and 9.4% for those aged 65 years and over; thus, exceeding the recommended threshold[footnote 4]. Amongst adults, men aged 75 years and over had the highest mean intake at 10.9% of total energy[footnote 4].
Some encouraging dietary trends have been emerging. National research suggests that the intake of free sugars is reducing over time in children (less so in adults), although it remains above recommended thresholds (no more than 5% of total energy)[footnote 5]. Fewer children and young people report drinking sugar-sweetened beverages, and those drinking them are consuming less[footnote 5]. Nonetheless, they remain a significant source of sugar and it should be noted that they get most of their free sugars intake from the foods presented in Figure 10.2 below and on NHS – Change4Life, most of which have little nutritional value.
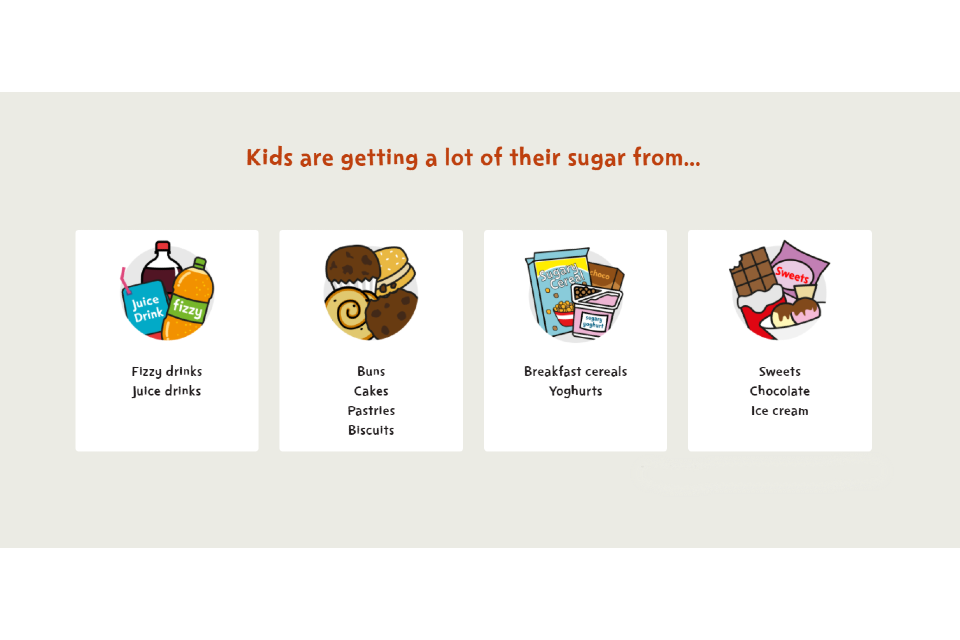
Figure 10.2. Common sources of free sugar in the diet of children and young people. Data from the National Diet and Nutrition Survey, 2018. Source (2)
The main sources of free sugars consumed by children are:
- soft drinks and fruit drinks
- cereal and cereal products
- sugar, preserves and confectionery[footnote 6]
In contrast there has been little change in the intake of fruit and vegetables over the past decade which provide a healthy alternative to free sugars. All age and sex groups have an average intake of fruit and vegetables below the minimum recommendation of having ‘At least 5 A Day’[footnote 5]. Thus, healthier eating advice should routinely be provided to promote good oral and general health for patients.
The main impact of the consumption of sugar-containing foods and drinks to oral health is dental caries in both adults and children; however, there is some evidence of dietary links with tooth wear and cancers.
Sugar consumption and dental caries
Sugar intake and the frequency of intake of sugars is particularly relevant for dental caries. The Stephan curve of pH in the oral cavity demonstrates why frequency is important. It illustrates how demineralisation (area coloured yellow) of tooth surfaces occurs after every sugar intake and the subsequent drop in pH that takes place in the mouth as oral bacteria convert sugar to acid (Figure 10.4a). This process stops as the buffering action of saliva returns the pH to normal (20 to 40 minutes). Saliva production varies across a 24-hour day, being stimulated at mealtimes whereas it is much reduced during sleep.
The impact of frequent sugar intakes is illustrated in Stephan’s curve in Figure 10.4b. In this case sugar intakes are experienced on many occasions during the day, so demineralisation occurs more often and the time between drops in pH is not long enough for effective remineralisation to take place. When sugar intakes are spaced some hours apart, there is a good opportunity for remineralisation, which is also more effective in the presence of fluoride.
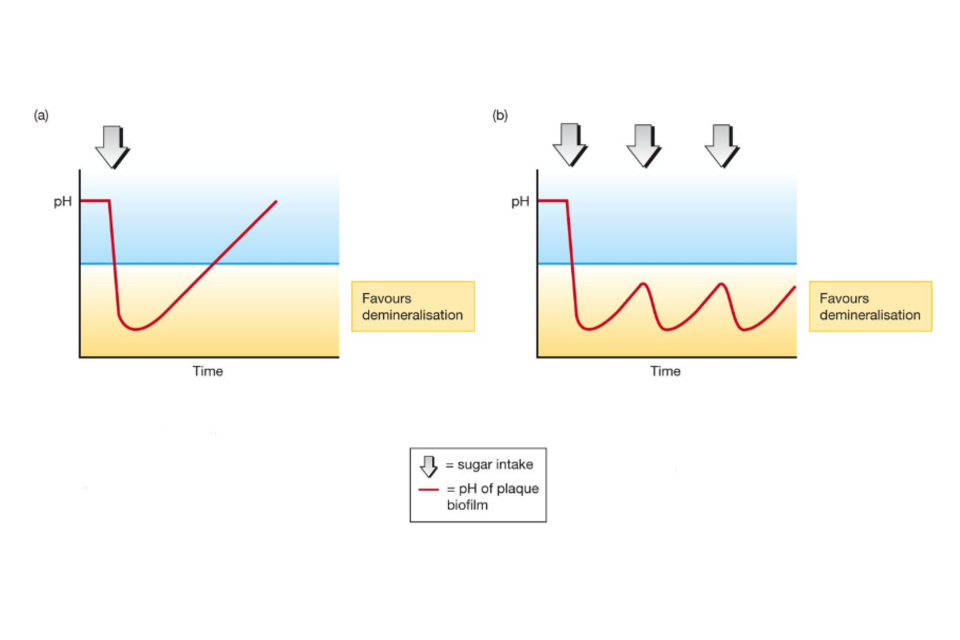
Figure 10.4. Effect of repeated sugars consumption on plaque biofilm pH. Reproduced from Chestnutt IG, Dental Public Health at a Glance, Wiley Blackwell, with permission. (a) The pH of fluid in the plaque biofilm falls rapidly on eating sugar (within one minute). Slowly recovers over 20 to 40 minutes as pH rises due to buffering and washing effect of saliva, sugar used up. (b) Repeated intakes of sugar mean that pH remains for prolonged period below the point which favours demineralisation.
Prospective cohort studies conducted in children and adolescents indicate that higher consumption (that is, the amount) of sugars, sugar-containing foods and sugar-sweetened beverages is associated with a greater risk of dental caries in the deciduous and permanent dentitions[footnote 1]. There is less available evidence on adults[footnote 7]. A higher frequency of consumption of free sugar-containing foods and beverages, but not total sugars, is also associated with greater risk of dental caries in the deciduous and permanent dentitions[footnote 1]. There is evidence that drinking sugar-sweetened beverages on a daily basis is related to greater dental caries risk in adults[footnote 8].
Recommendations to prevent tooth decay are as follows:
- minimise the amount and frequency of consumption of sugar-containing foods and drinks
- avoid sugar-containing foods and drinks at bedtime when saliva flow is reduced, and buffering capacity is reduced
All food and drink containing sugars should be consumed as part of a meal and not as a between-meal snack. It is important to recognise that honey, fruit smoothies, fresh fruit juice and dried fruit all contain cariogenic sugars and should not be consumed as a between-meal snack. Neither should fruit in sugary syrup. Fresh fruit (or alternatively frozen fruit, or fruit canned in juice) are recommended snacks between meals.
Fizzy drinks, soft drinks, juice drinks and squashes sweetened with sugar have no place in a child’s daily diet[footnote 1].
Most free sugars in the diet are contained in processed and manufactured foods and drinks. Consumers should check labels carefully to find out how much sugar a product contains. NHS Eatwell[footnote 9], Change4Life[footnote 10], and the Change4Life food scanner App are helpful resources.
Similar messages should be reinforced throughout life and this is particularly important as people enter later life when diet and health behaviours change, and risks increase under a variety of influences.
Diet and cancer
As a population, we would benefit from eating a variety of fruit and non-starchy vegetables, consuming at least 5 portions per day. Whilst there is evidence that those whose diets are low in fresh fruit and vegetables have a moderately increased risk of cancers in general[footnote 11], there is little evidence that poor diet is a risk factor for oral cancer, compared with using tobacco and particularly when tobacco and alcohol consumption are combined.
Diet and tooth wear
In general, patients should be encouraged to eat a healthy balanced diet. Only where there is evidence of tooth wear should possible dietary risk factors be identified and patients advised to reduce the frequency of intake of acidic foods or drinks; keep acidic food and drinks to mealtimes and explore alternatives, particularly between meals. It is also important to advise against methods of drinking that promote tooth wear such as swilling and swishing.
General good dietary practice guidelines
Below are some of the main healthy eating messages aimed at helping people make healthier dietary choices.
The 2 most important elements of a healthy diet include:
- eating the right amount of food, relative to how active a person is to be a healthy weight
- eating a range of different types of foods in line with the Eatwell Guide
The Eatwell Guide[footnote 12] is a key tool that defines the government’s recommendations on a healthy diet for children and adults. Of note the guide contains lots of flexibility for culturally diverse foods. It does not apply to children under 2 years of age because they have different nutritional needs. Furthermore, between the ages of 2 and 5 years, children should gradually move to eating the same foods as the rest of the family, in proportions shown in the Eatwell Guide. It makes healthy eating easier to understand by providing a visual representation of the proportions in which different types of foods are needed to have a well-balanced and healthy diet. The proportions shown are representative of food consumption over the period of a day, or even a week, not necessarily each mealtime. A balanced diet contains foods from all 5 major food groups.
The Eatwell Guide encourages us to:
- eat at least 5 portions of a variety of fruit and vegetables every day
- base meals on potatoes, bread, rice, pasta and other starchy carbohydrates, choosing wholegrain versions where possible
- have some dairy or dairy alternatives (such as soy drinks); choosing lower fat and lower sugar options
- eat some beans, pulses, fish, eggs, meat and other proteins (including 2 portions of fish every week, 1 of which should be oily)
- choose unsaturated oils and spreads and eat in small amounts
- drink 6 to 8 cups or glasses of fluid a day
- if consuming foods and drinks high in fat, salt or sugar, have these less often and in small amounts
Key messages for a healthier diet
Whilst those at higher risk of disease may require specific advice, everyone has the potential to benefit from a healthier diet. You may find it helpful to refer patients to the Eatwell Guide booklet, which is available online, as this can be emailed to patients[footnote 13].
Eat at least 5 portions of a variety of fruit and vegetables every day
Eat at least 5 portions of a variety of fruit and non-starchy vegetables every day. Starchy vegetables such as potatoes only count towards carbohydrate intake. A portion of fruit or vegetables is 80g. Fresh, frozen, canned, dried and juiced all count. One portion of dried fruit is only 30g which could be 3 dried apricots or one tablespoon of raisins. It is important to limit fruit juice and smoothies to a combined total of 150ml per day. Just one portion of fruit juice or smoothie (150ml) counts as one of (at least) 5-a-day.
There is evidence to suggest that people who eat lots of fruit and vegetables are less likely to develop chronic diseases such as coronary heart disease and some types of cancer.
Potatoes, bread, rice, pasta and other starchy carbohydrates
Base meals on starchy carbohydrates, including potatoes, bread, rice and pasta. Choose wholegrain varieties, or keep the skins on potatoes, for more fibre, vitamins and minerals.
Dairy and alternatives
Eat some dairy or dairy alternatives but choose lower fat options when possible. For products such as yoghurt, people should be encouraged to check the label and choose those lower in fat and sugars.
Beans, pulses, fish, eggs, meat and other proteins
Eat some beans, pulses, fish, eggs, meat and other proteins. Eat at least 2 portions (2 x 140g) of fish each week, one of which is oily. Limit processed meats such as sausages, bacon and cured meats. People who eat more than 90g per day of red or processed meats should try to reduce the amount to no more than an average of 70g per day.
Oils and spreads
People should be encouraged to use these products sparingly as they are high in fat. Cutting down on these types of foods could help to control your weight as they are high in calories.
Foods high in fat, salt and sugar
These foods are not required as part of a healthy, balanced diet. If included, they should only be consumed infrequently and in small amounts. Most people need to cut down on the amount of high fat, salt and sugar-containing foods and drinks consumed.
Cut down on saturated fat
Cutting down on saturated fat can lower blood cholesterol and reduce the risk of heart disease. Most people in the UK eat too much saturated fat. An average man should have no more than 30g saturated fat a day. The average woman should have no more than 20g saturated fat a day. Children should have less saturated fat than adults. A low-fat diet is not suitable for children under 5 years.
One of the easiest ways to cut down on saturated fat is to compare the labels on similar products and choose the one lower in saturated fat. Patients should be encouraged to watch out for foods that are high in saturated fat, including fatty cuts of meat, sausages, butter, cream, cheese, chocolate, pastries, cakes and biscuits. It is not necessary to stop eating these foods altogether; but eating too much of these can result in people having more than the recommended maximum amount of saturated fat.
Cut down on the amount and frequency of sugar containing foods and drinks
As stated earlier in this chapter, recommendations in order to reduce dental caries advocate minimising or reducing the amount and frequency of sugar-containing foods and drinks. Regularly consuming foods and drinks high in free sugars increases the risk of dental caries and obesity. Ideally, no more than 5% of total energy intake should come from free sugars.
All patients and, in the case of children, their parents, are encouraged to ‘sugar swap’. It is particularly helpful to swap drinks containing free sugars for water, lower fat milk or sugar-free alternatives, including tea and coffee. Alcohol has a high calorific content and limiting its intake to within 14 units per week helps keep health risks low for both men and women[footnote 14]. When advising adults, do also highlight the sugar and calories in alcoholic as well as non-alcoholic drinks.
Cut down on salt
Eating too much salt can raise blood pressure, which increases the risk of developing heart disease or stroke. Adults should eat no more than 6g of salt a day (6g of salt is about a teaspoonful) and children should have less salt. Most of the salt eaten is already in everyday foods such as bread, breakfast cereal, pasta sauce, soups and starchy snacks.
Drink plenty of fluids
Drinking about 6 to 8 glasses of fluids every day is recommended to prevent dehydration. Water, lower fat milk and sugar-free drinks including tea and coffee all count. Fruit juices and smoothies count towards fluid consumption but are a source of free sugars and so consumption should be limited to no more than a combined total of 150 ml a day and consumption with meals should be recommended.
Changing to a healthier diet
There is very little reliable evidence available to draw conclusions about the effects of dietary interventions in the dental setting for reducing sugar consumption or making other beneficial dietary changes. This reflects the paucity of high quality research in the field; however, more promising results are emerging as outlined below:
-
A systematic review suggests interactive dietary counselling with 11 to 12 year olds may increase their use of xylitol products[footnote 15], as an alternative to free sugar.
-
A trial involving a tailored 30-minuted structured conversation with parents and children (5 to 7 year olds) who required extraction of primary teeth due to dental caries, achieved promising results in caries management[footnote 16]. This trial, informed by motivational interviewing, aiming to prevent future dental caries, involved setting preventive goals and having a review appointment with the child’s general dental practitioner, who was advised to treat the child as being at high dental caries risk[footnote 16].
When giving dietary advice to minimise consumption of sugars, it is good practice to assess the overall pattern of eating to establish the following information:
- the number of intakes of food and drinks per day
- the number of intakes that contain sugars and how many were consumed between normal mealtimes
- whether any intakes containing sugars were taken before bedtime – this is important as reduced salivary flow overnight reduces dental caries protective effects
An example of one type of diary is available to download.
Overall, it is important to use contemporary theory and evidence on behaviour change in general to inform preventive practice as explored further in Chapter 3. A diet modification approach should be used in conjunction with actions to increase fluoride availability. However, lowering the amount and frequency of free sugars consumed will have wider health benefits, preventing weight gain and obesity which in turn will reduce the risk of heart disease, type 2 diabetes and some cancers.
Diet in the early years
Breastfeeding
Breastfeeding makes an important contribution to infant and lifelong health and represents the physiological norm for infant feeding for around the first 6 months of life. It provides the best start in life and continuing breastfeeding beyond 6 months has beneficial effects for both mother and child. The additional benefits for infants include a reduced risk of dental caries[footnote 17][footnote 18][footnote 19], and being less likely to develop malocclusions compared with ‘never breastfed’ children[footnote 20].
Infants should be exclusively breastfed for around the first 6 months of life[footnote 21] (Chapter 2: Table 1). The available evidence indicates that breastfeeding up to 12 months of age is associated with a decreased risk of dental caries and may offer some protection when compared with infant formula[footnote 18]. The evidence on breastfeeding after one year is not straightforward because much of the research is observational and does not adjust for confounders such as dietary factors, oral hygiene practices and use of fluoride containing products. Further well-designed research is needed[footnote 17][footnote 22].
Once teeth begin to appear, parents may raise the dilemma of when to brush a child’s teeth if they fall asleep at the breast. Parents should be encouraged to brush children’s teeth as close to bedtime as possible and follow the general guidelines, rather than wake a child to brush their teeth.
Bottle feeding
Families may choose to bottle feed their babies or mothers may be unable to breastfeed. They should be supported if, after being given advice, information and support, they opt to bottle feed using formula milk. Only breast milk, infant formula or cooled boiled water should be given in a bottle. Sugar, honey or any other sugar-containing products or drinks must not be added to bottles. From the age of 6 months babies should be encouraged to drink from a free-flow cup (rather than one with a valve which requires a child to suck) and feeding from a bottle should be discouraged from the age of one year[footnote 20].
Infant feeding: Moving on to solids
Children’s food preferences and eating habits are formed early in life and so it is important to support the development of healthy eating habits in young children. From around 6 months, infants should be introduced to a wide range of foods, including iron-containing foods, in an age-appropriate form and at a time and in a manner to suit both family and individual child[footnote 13]. The transition to include solid foods should occur when infants are developmentally ready. Solids should be introduced alongside continued breastfeeding or infant formula; these, and water, should be the only drinks offered as infants move on to solids[footnote 20].
A wide variety of solid foods with different flavours and textures should gradually be introduced to diversify the infant diet and to help ensure nutritional requirements are met. Examples of first solid foods include blended, mashed, or soft-cooked vegetables (for example parsnip, broccoli, potato, yam, sweet potato, carrot) and fruit (for example apple or pear). Batons (sticks) of vegetables provide healthy ‘finger food’ as children begin to feed themselves. Example menus for early years settings provide lots of practical menu suggestions[footnote 24], along with the Start4Life website[footnote 25]. It is important to encourage parents to try a range of healthy foods with children to find which ones they enjoy. This way parents can establish the basis of healthy eating in life.
Commercial baby foods
Commercial baby foods and drinks aimed at children up to 36 months may provide infants’ first non-milk taste experiences and form a substantial proportion of their diet. Labelling may be confusing for parents particularly when the terms natural or organic sugars are used – they are still cariogenic. A recent review found that there are inconsistencies between national recommendations on infant and young child feeding and the types of products available, their ingredients, nutrition composition and product labelling and marketing[footnote 26].
Some commercial baby foods have added sugar or salt or contain ingredients that are high in sugar or salt. This is more common in commercial baby finger-foods, which are often marketed as snacks. Sweet finger foods (including biscuits, wafers, puffs, bars, bites, fruit shapes) make up two-thirds of the baby finger-food market.
The highest sugar content is found in processed dried fruit products, which are often marketed as ‘healthy snacks’ due to their fruit content, but the sugar in these products is often free sugars as they contain ingredients such as fruit juices, purees and concentrates.
Fruit and vegetables are recommended first foods for infants and young children. Advice is to start feeding infants with single vegetables and fruits, and vegetables that are less sweet. However, the balance of products on the market is mainly fruit, particularly mixed fruit; a less sweet product mix would better prepare babies to accept a wide range of different, less sweet tastes and protect dental health.
More than one-third of baby meals are marketed at children under 6 months, despite government advice that solid foods should be introduced (alongside breast milk or infant formula) at around 6 months of age.
Nearly three-quarters of fruit juice-based baby drinks are marketed at infants under 12 months, which is inconsistent with advice to offer only breast milk, infant formula or water as drinks between 6 and 12 months of age.
Source: Public Health England (2019)[footnote 26].
Feeding patterns and practices
Feeding practices are continually changing and raise questions for the oral healthcare team. When new products are introduced, you may be required to give advice on products and practices for which there is not specific research evidence. As a helpful guide, it is worth reflecting on their sugar content and the principles of sugar frequency and consumption. Recent examples which encourage grazing include ‘nets’ or ‘pacifier-type’ feeding devices into which carers insert selected foods. Commercially produced ‘pouches’ of food are increasingly common. Around one-third of commercial baby foods and drinks are packaged in pouches, many of which have nozzles[footnote 26]. Although some companies provide advice (on the back of the pack or website) on how to feed these products (from a spoon), this is not consistent across the market. Whilst there is no specific research evidence of the impact for developing teeth it is likely that these foods can be consumed ‘on the go’ and over longer periods of time; therefore, having prolonged contact with teeth and, if sugar containing, more likely to increase the risk of dental caries. It is increasingly important to discuss how products are consumed as well as their sugar content.
Bedtime routines
The importance of bedtime routines and defining what constitutes a bedtime routine have recently been the subject of professional deliberations and research[footnote 27][footnote 28]. The frequency and amount of food and drinks containing free sugars should be as low as possible in the first year of life[footnote 20]. Only plain milk or water should be provided between meals for young children and baby juices or sugary drinks discouraged, particularly at bedtime[footnote 20]. A recent systematic review confirms a consistent positive association between caries risk and free sugars ingestion around bedtime across three age-groups (3 to 5 years, 6 to 11 years, 12 to 16 years)[footnote 28]. The certainty of evidence was very low and that is perhaps not surprising, given the challenges of conducting this type of research. However, the recommendation to avoid food and drinks containing free sugars before bedtime in children, (and, of course, overnight), is based on a sound physiology and good practice for everyone.
Teething
A variety of interventions, gels and solutions are used by parents to manage teething, generally unsupported by clinical evidence[footnote 29]. However, it is important to note that some teething products may include sugar[footnote 29] and the Medicines and Healthcare products Regulatory Agency (MHRA) has ensured that products should carry this warning[footnote 29]. There is helpful information for parents on the NHS website on a range of methods to manage teething including teething rings, painkillers, breadsticks and fresh fruit or vegetable sticks. Tips for helping your teething baby.
Vulnerable groups
Dietary advice for vulnerable groups experiencing medical, physical and mental health challenges needs to be tailored to their specific circumstances (Chapter 4) and may involve close working with colleagues across health and social care. It may require greater use of protective factors including fluoride (Chapter 9).
Resources
Start4Life: trusted NHS help and advice during pregnancy, birth and parenthood. Includes content on breastfeeding and weaning.
Change4Life: easy ways to eat well and move more. Includes content on sugar swaps for kids, food labelling and quick and easy snack ideas.
Feeding in the first year of life: SACN report.
Commercial infant and baby food and drink: evidence review: a report setting out the evidence for action on food and drink product ranges targeted at babies and young children, and Public Health England (PHE)’s advice to government.
Infant feeding: information to support the commissioning of local infant feeding services.
NHS: tips for helping your teething baby.
NHS: What to feed young children.
Example menus for early years settings in England: example menus and useful guidance for early years settings to help meet the Early Years Foundation Stage requirements for food and drink.
PHE: Sugar Reduction Programme: progress made by industry in the first year. Includes a suite of sugar and calorie reduction infographics.
References
-
SACN. Carbohydrates and health. London: TSO; 2015. ↩ ↩2 ↩3 ↩4 ↩5
-
Swan GE, Powell NA, Knowles BL, Bush MT, Levy LB. A definition of free sugars for the UK. Public Health Nutrition. 2018;21(9):1636-8. ↩
-
Public Health England. National Diet and Nutrition Survey. London: Public Health England; 2020. ↩ ↩2 ↩3 ↩4
-
Public Health England, Food Standards Agency, NatCen, MRC. National Diet and Nutrition Survey: Years 1 to 9 of the Rolling Programme (2008/2009 to 2016/2017): Time trend and income analyses. London: Public Health England; 2019. ↩ ↩2 ↩3
-
Public Health England, Food Standards Agency, NatCen, MRC. National Diet and Nutrition Survey: results from years 7 and 8 (combined). London: Public Health England; 11 April 2018. ↩
-
Bernabé E, Vehkalahti MM, Sheiham A, Lundqvist A, Suominen AL. The Shape of the Dose-Response Relationship between Sugars and Caries in Adults. Journal of Dental Research. 2016;95(2):167-72. ↩
-
Bernabé E, Vehkalahti MM, Sheiham A, Aromaa A, Suominen AL. Sugar-sweetened beverages and dental caries in adults: a 4-year prospective study. Journal of Dentistry. 2014;42(8):952-8. ↩
-
NHS. Eat well: Sugar the facts. London: NHS; 2018 [updated 29 January 2019]. ↩
-
NHS. Change4Life. London: NHS; 2020. ↩
-
Walsh T, Liu JLY, Brocklehurst P, Glenny AM, Lingen M, Kerr AR and others. Clinical assessment to screen for the detection of oral cavity cancer and potentially malignant disorders in apparently healthy adults. Cochrane Database of Systematic Reviews. 2013(11). ↩
-
Public Health England. The Eatwell Guide. London: Public Health England; 2016. ↩
-
Public Health England. The Eatwell Guide booklet. London: Public Health England; 2016. ↩ ↩2
-
UK Chief Medical Officers’. UK Chief Medical Officers’ Low Risk Drinking Guidelines 2016. London: Department of Health England, Welsh Government, Department of Health Ireland, Scottish Government; 2016 25.08.2016. ↩
-
Harris R, Gamboa A, Dailey Y, Ashcroft A. One‐to‐one dietary interventions undertaken in a dental setting to change dietary behaviour. Cochrane Database of Systematic Reviews. 2012(3). ↩
-
Pine CM, Adair PM, Burnside G, Brennan L, Sutton L, Edwards RT and others. Dental RECUR Randomized Trial to Prevent Caries Recurrence in Children. Journal of Dental Research. 2020;99(2):168-74. ↩ ↩2
-
Tham R, Bowatte G, Dharmage SC, Tan DJ, Lau MX, Dai X and others. Breastfeeding and the risk of dental caries: a systematic review and meta-analysis. Acta Paediatricia. 2015;104(467):62-84. ↩ ↩2
-
Avila WM, Pordeus IA, Paiva SM, Martins CC. Breast and Bottle Feeding as Risk Factors for Dental Caries: A Systematic Review and Meta-Analysis. PLoS One. 2015;10(11):e0142922. ↩ ↩2
-
Cui L, Li X, Tian Y, Bao J, Wang L, Xu D and others. Breastfeeding and early childhood caries: a meta-analysis of observational studies. Asia Pacific Journal of Clinal Nutrition. 2017;26(5):867-80. ↩
-
SACN. Scientific Advisory Committee on Nutrition (SACN) Feeding in the first year of life. London: TSO; 2018. ↩ ↩2 ↩3 ↩4 ↩5
-
World Health Organization. Breastfeeding. Geneva: WHO; 2019. ↩
-
Peres KG, Nascimento GG, Peres MA, Mittinty MN, Demarco FF, Santos IS and others. Impact of Prolonged Breastfeeding on Dental Caries: A Population-Based Birth Cohort Study. Pediatrics. 2017;140(1). ↩
-
HM Government. Examples Menus for Early Years Settings. London; 2017. ↩
-
NHS. Start4Life. London: NHS; 2020. ↩
-
Public Health England. Commercial infant and baby food and drink: evidence review. London: PHE; 2019. ↩ ↩2 ↩3
-
Kitsaras G, Goodwin M, Allan J, Pretty IA. Defining and measuring bedtime routines in families with young children – A DELPHI process for reaching wider consensus. PLOS ONE. 2021;16(2):e0247490. ↩
-
Baghlaf K, Muirhead V, Moynihan P, Weston-Price S, Pine C. Free Sugars Consumption around Bedtime and Dental Caries in Children: A Systematic Review. Journal of Dental Research Clinical Translational Research. 2018;3(2):118-29. ↩ ↩2
-
Monaghan N. Teething issues. British Dental Journal. 2019;227(10):883. ↩ ↩2 ↩3
